For US Healthcare Professionals
Actor portrayal
Actor portrayal
Make diagnosing kidney stone disease easier
Make diagnosing kidney stone disease easier
For pediatric patients <18 years of age with a single stone or anyone experiencing recurrent kidney stones (RKS):
For pediatric patients <18 years of age with a single stone or anyone experiencing recurrent kidney stones (RKS):
- Diagnosing the underlying causes can be complicated by the rarity of associated hereditary conditions, wide clinical variability, and overlapping symptoms of other genetic kidney stone disorders.1,2
- Underlying causes of RKS often go undiagnosed, which can result in progressive damage to the kidneys, leading to chronic kidney disease (CKD) and eventually end-stage kidney disease (ESKD).1-3
- Delays in diagnosis can be detrimental.2,4
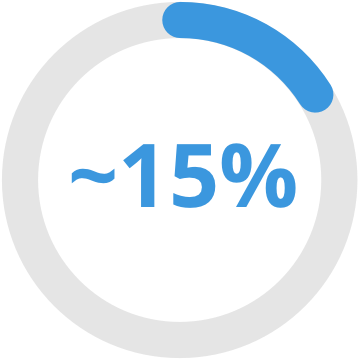
In a study of patients with nephrolithiasis/nephrocalcinosis, ~15% had a causative monogenic condition5
of patients with nephrolithiasis/
nephrocalcinosis had a causative monogenic condition5
Studies have shown that children with nephrolithiasis have as high as 50% risk of recurrence within 3 years following a kidney stone event.6
Studies have shown that children with nephrolithiasis have as high as 50% risk of recurrence within 3 years following a kidney stone event.6
Know the value of genetic testing for kidney stone disease

Gene-specific analysis can be pivotal for accurate diagnosis due to symptomatic overlap in the clinical presentation of patients with kidney stone diseases.7
Identifying disease-causing mutations can allow for patient management that may reduce recurrent symptoms or progression to ESKD.8

Learn about the NovoDETECT™ genetic testing program at NovoDETECT.com to get started with uncovering the underlying genetic cause of early-onset kidney stones or RKS.
Consider a condition like primary hyperoxaluria
Consider a condition like primary hyperoxaluria
Many patients with primary hyperoxaluria experience a significant delay from initial symptom onset to diagnosis10-12
Many patients with primary hyperoxaluria experience a significant delay from initial symptom onset to diagnosis10-12
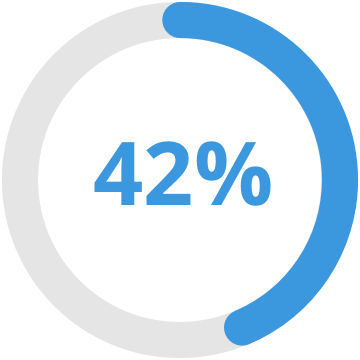
In a study, 42% of patients with PH experienced a significant delay in diagnosis10
Patients experienced 3.4 ± 5.4 years between first symptom presentation and diagnosis10
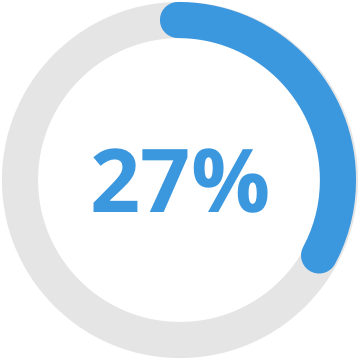
One study reported that 27% of patients were diagnosed at ESRD, with delay of 3.5 years after symptom onset11
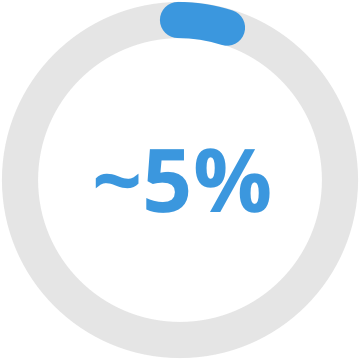
A separate study found that ~5% were diagnosed after kidney transplant12
19% diagnosed after transplant were not diagnosed until after first transplant failure12
Diagnosis typically begins with 24-hour urine collection and kidney stone analysis13
Diagnosis typically begins with 24-hour urine collection and kidney stone analysis13
Urine collection
(eGFR>30mL/min/1.73m14)14
24-hour urine collection (preferred):
Elevated Uox on at least 2 assessments, >0.7mmol (64mg)/24 h14
Spot urine collection:
Oxalate: creatinine ratio > normal for age
Plasma collection (eGFR <30mL/min/1.73m14)14,15:
Plasma oxalate > 20 µmol/L
Stone analysis13,14:
- PH1: Characteristic morphology and >95% CaOx monohydrate
- PH2 and PH3: Stone burden and speed of recurrence
Additional urinary metabolite measures (nonconfirmatory)13,14,16:
- Elevated glycolate may indicate PH1
- Elevated glycerate may indicate PH2
- Elevated HOG may indicate PH3
Abbreviations: CaOx=calcium oxalate; eGFR=estimated glomerular filtration rate; HOG=4-hydroxy-2-oxoglutarate; Uox=urinary oxalate.
Rule out secondary causes14,15
- Enteric causes (eg, chronic pancreatitis, cystic fibrosis, inflammatory bowel syndrome, bariatric surgery)
- Very high-oxalate, low-calcium diet
- Infant with prematurity
Genetic testing for known mutations14,15
- AGXT mutations: PH1
- GRPHR mutations: PH2
- HOGA1 mutations: PH3
The order of testing is based on clinical judgement.
*Urinary oxalate >0.5 mmol/1.73 m2/24 hours and/or plasma oxalate >20 µmol/L.5
A definitive diagnosis of primary hyperoxaluria requires genetic testing3,9
Patients with primary hyperoxaluria present with certain characteristics. For both pediatric and adult patients, these characteristics may include a history of kidney stones or nephrocalcinosis, a family history of hyperoxaluria, or chronic kidney disease, defined as a glomerular filtration rate (GFR) of <50 mL/min/1.73 m2 or a serum creatinine ≥2 times normal for age.15,18-19
Screening for primary hyperoxaluria should be undertaken in a child with a first kidney stone, in an adult with recurrent kidney stones, and in patients with nephrocalcinosis or a family history of kidney stones.13
Visit NovoDETECT™ to learn more about genetic testing for genetic kidney stone disease, including PH.
References
- Monico CG, Milliner DS. Genetic determinants of urolithiasis. Nat Rev Nephrol. 2011;8(3):151-162.
- Ferraro PM, D’Addessi A, Gambaro G. When to suspect a genetic disorder in a patient with renal stones, and why. Nephrol Dial Transplant. 2013;28(4):811-820.
- Milliner DS, Harris PC, Sas DJ, et al. Primary hyperoxaluria type 1. GeneReviews®. 2022. Published February 10, 2022. Accessed September 8, 2023. https://www.ncbi.nlm.nih.gov/books/NBK1283
- Edvardsson VO, Goldfarb DS, Lieske JC, et al. Hereditary causes of kidney stones and chronic kidney disease. Pediatr Nephrol. 2013;28(10):1923-1942.
- Halbritter J, Seidel A, Müller L, et al. Update on hereditary kidney stone disease and introduction of a new clinical patient registry in Germany. Front Pediatr. 2018;6:47. doi: 10.3389/fped.2018.00047
- Medairos R, Paloian NJ, Pan A, et al. Risk factors for subsequent stone events in pediatric nephrolithiasis: a multi-institutional analysis. J Pediatr Urol. 2022;18(1):26.e1-26.e9. doi: 10.1016/j.jpurol.2021.11.012
- Cogal AG, Arroyo J, Shah RJ, et al. Comprehensive genetic analysis reveals complexity of monogenic urinary stone disease. Kidney Int Rep. 2021;6(11):2862-2884.
- Braun DA, Lawson JA, Gee HY, et al. Prevalence of monogenic causes in pediatric patients with nephrolithiasis or nephrocalcinosis. Clin J Am Soc Nephrol. 2016;11(4):664-672.
- Ben-Shalom E, Frishberg Y. Primary hyperoxalurias: diagnosis and treatment. Pediatr Nephrol. 2105;30(10):1781-1791.
- Hoppe B, Langman C. A United States survey on diagnosis, treatment, and outcome of primary hyperoxaluria. Pediatr Nephrol. 2003;18(10):986-991.
- Zhao F et al. Predictors of incident esrd among patients with primary hyperoxaluria presenting prior to kidney failure. Clin J Am Soc Nephrol. 2016;11(1):119-126.
- Bergstralh EJ et al. Transplantation outcomes in primary hyperoxaluria. Am J Transplant. 2010;10(11):2493-2501.
- Cochat P, Rumsby G. Primary hyperoxaluria. N Engl J Med. 2013;369(7):649-658.
- Groothoff JW et al. Clinical practice recommendations for primary hyperoxaluria: an expert consensus statement from ERKNet and OxalEurope. Nat Rev Nephrol. 2023;19(3):194-211.
- Edvardsson VO et al. Pediatr Nephrol. 2013;28(10):1923-1942.
- Sas DJ et al. Recent advances in the identification and management of inherited hyperoxalurias. Urolithiasis. 2019;47(1):79-89.
- Test ID: CYSQN. Cystinuria profile, quantitative, 24-hour, urine: clinical and interpretive. Mayo Clinic Laboratories. Accessed August 4, 2020. https://www.mayocliniclabs.com/test-catalog/Clinical+and+Interpretive/8376
- Nephrocalcinosis. Dorland’s Illustrated Medical Dictionary. 33rd ed. Elsevier; 2019. Accessed May 12, 2020. https://www.dorlandsonline.com/dorland/definition?id=33496
- Hyperoxaluria. Dorland’s Illustrated Medical Dictionary. 33rd ed. Elsevier; 2019. Accessed May 12, 2020. https://www.dorlandsonline.com/dorland/definition?id=23930

