For US Healthcare Professionals
Warning signs of primary hyperoxaluria
Actor portrayal
Warning signs of primary hyperoxaluria
Patient warning signs can include one or a combination of the symptoms listed below1-7:
Patient warning signs can include one or a combination of the symptoms listed below1-7:
A single kidney stone in children or recurring kidney stones in adults should cause suspicion of primary hyperoxaluria (PH).
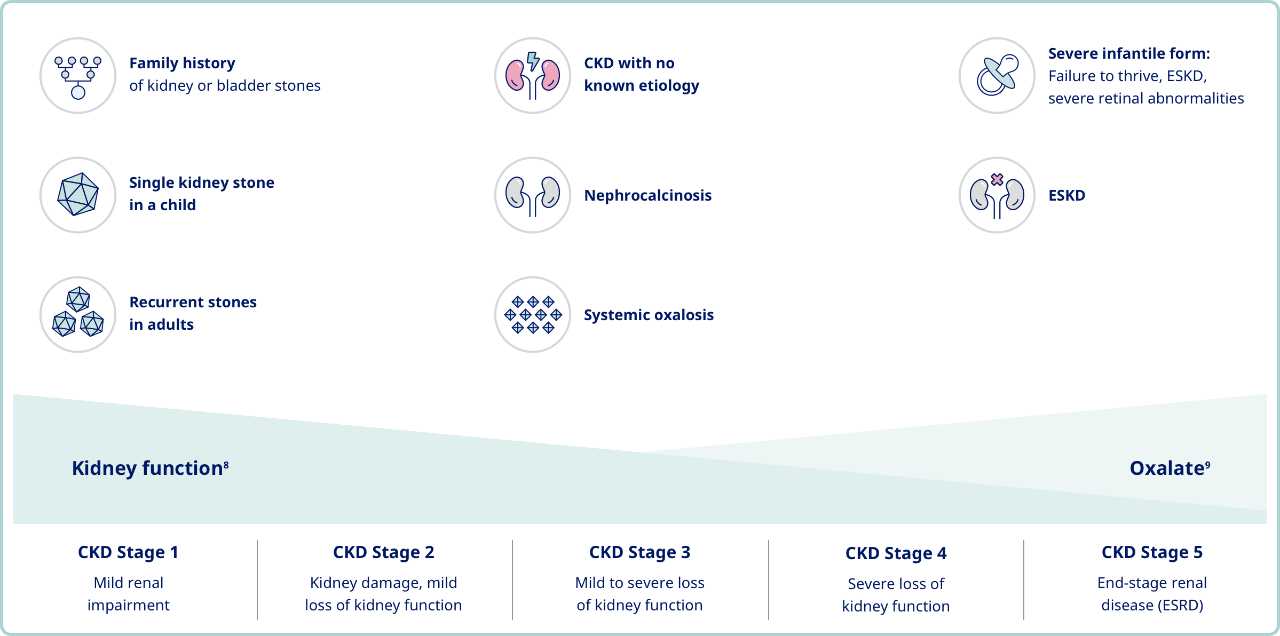
Family history of kidney or bladder stones
Many patients are asymptomatic for years, with 18% of people with primary hyperoxaluria type 1 being diagnosed by familial screening before they show any symptoms.5,7

A single pediatric kidney stone
Children should not develop bladder or kidney stones, and the presence of even a single kidney stone in an infant or child should immediately raise suspicion of a genetic condition like primary hyperoxaluria.2,10
Recurring kidney stones in adults
A single kidney stone in an adult is not uncommon, but recurring kidney stones can be indications of an underlying metabolic disorder or genetic disease.2,10
Chronic kidney disease (CKD) with unknown etiology
Suspect primary hyperoxaluria when a patient presents with reduced renal function combined with nephrocalcinosis or a high occurrence of kidney stones.1,9,13
Nephrocalcinosis
Both pediatric and adult patients with early signs of nephrocalcinosis should be screened for primary hyperoxaluria.2,10
Systemic oxalosis
Kidney failure can be the first clinical indication of primary hyperoxaluria in some patients, even in infancy. When patients are in kidney failure, calcium oxalate can deposit in tissues throughout the body.9,14
Systemic oxalosis can also impact bone, skin, heart, and eye health.14,15
Failure to thrive, ESRD, severe retinal abnormalities, or vision loss in infants
In a study, infantile onset was shown to occur in 18% of patients with PH1. Infants with this severe form present with end-stage kidney disease, failure to thrive, severe retinal abnormalities, and vision loss during their first year.3,4,6,16
End-stage renal disease (ESRD)
Studies have shown that many people are not diagnosed with PH until they are in ESRD (35% of all patients with PH1 and 11% of patients with PH2), although these patients often had earlier symptoms that went unrecognized, such as recurring kidney stones. 59% to 70% of people diagnosed with PH1 as adults are in ESRD at the time of diagnosis.3,4,7,17-18
Learn more about diagnosing primary hyperoxaluria
References
- Edvardsson VO et al. Hereditary causes of kidney stones and chronic kidney disease. Pediatr Nephrol. 2013;28(10):1923-194.
- Bhasin B et al. Primary and secondary hyperoxaluria: understanding the enigma. World J Nephrol. 2015;4(2):235-244.
- Harambat J et al. Genotype-phenotype correlation in primary hyperoxaluria type 1: the p.Gly170Arg AGXT mutation is associated with a better outcome. Kidney Int. 2010;77(5):443-449.
- van Woerden CS et al. Primary hyperoxaluria type 1 in The Netherlands: prevalence and outcome. Nephrol Dial Transplant. 2003;18(2):273-279.
- Frishberg Y et al. Intra-familial clinical heterogeneity: absence of genotype-phenotype correlation in primary hyperoxaluria type 1 in Israel. Am J Nephrol. 2005;25(3):269-275.
- Birtel J et al. The ocular phenotype in primary hyperoxaluria type 1. Am J Ophthalmol. 2019;206:184-191.
- Mandrile G et al. Data from a large European study indicate that the outcome of primary hyperoxaluria type 1 correlates with the AGXT mutation type. Kidney Int. 2014;86(6):1197-1204.
- National Kidney Foundation. Estimated glomerular filtration rate (eGFR). Published 2018. Accessed February 12, 2020. https://www.kidney.org/atoz/content/gfr
- Milliner DS. The primary hyperoxalurias: an algorithm for diagnosis. Am J Nephrol. 2005;25(2):154-160.
- Cochat P et al. Primary hyperoxaluria Type 1: indications for screening and guidance for diagnosis and treatment. Nephrol Dial Transplant. 2012;27(5):1729-1736.
- Marra G et al. Pediatric nephrolithiasis: a systematic approach from diagnosis to treatment. J Nephrol. 2019;32(2):199-210.
- National Institute of Diabetes and Digestive and Kidney Diseases. Symptoms & causes of kidney stones in children. Published May 2017. Accessed September 2, 2020. https://www.niddk.nih.gov/health-information/urologic-diseases/kidney-stones-children/symptoms-causes
- Milliner DS et al. Primary hyperoxaluria type 3. GeneReviews®. University of Washington, Seattle; 2015.
- Sas DJ et al. Recent advances in the identification and management of inherited hyperoxalurias. Urolithiasis. 2019;47(1):79-89.
- Salido E et al. Primary hyperoxalurias: disorders of glyoxylate detoxification. Biochim Biophys Acta. 2012;1822(9):1453-1464.
- Soliman NA et al. Clinical spectrum of primary hyperoxaluria type 1: experience of a tertiary center. Nephrol Ther. 2017;13(3):176-182.
- Zhao F et al. Predictors of incident ESRD among patients with primary hyperoxaluria presenting prior to kidney failure. Clin J Am Soc Nephrol. 2016;11(1):119-126.
- Garrelfs SF et al. Patients with primary hyperoxaluria type 2 have significant morbidity and require careful follow-up. Kidney Int. 2019;96(6):1389-1399.

